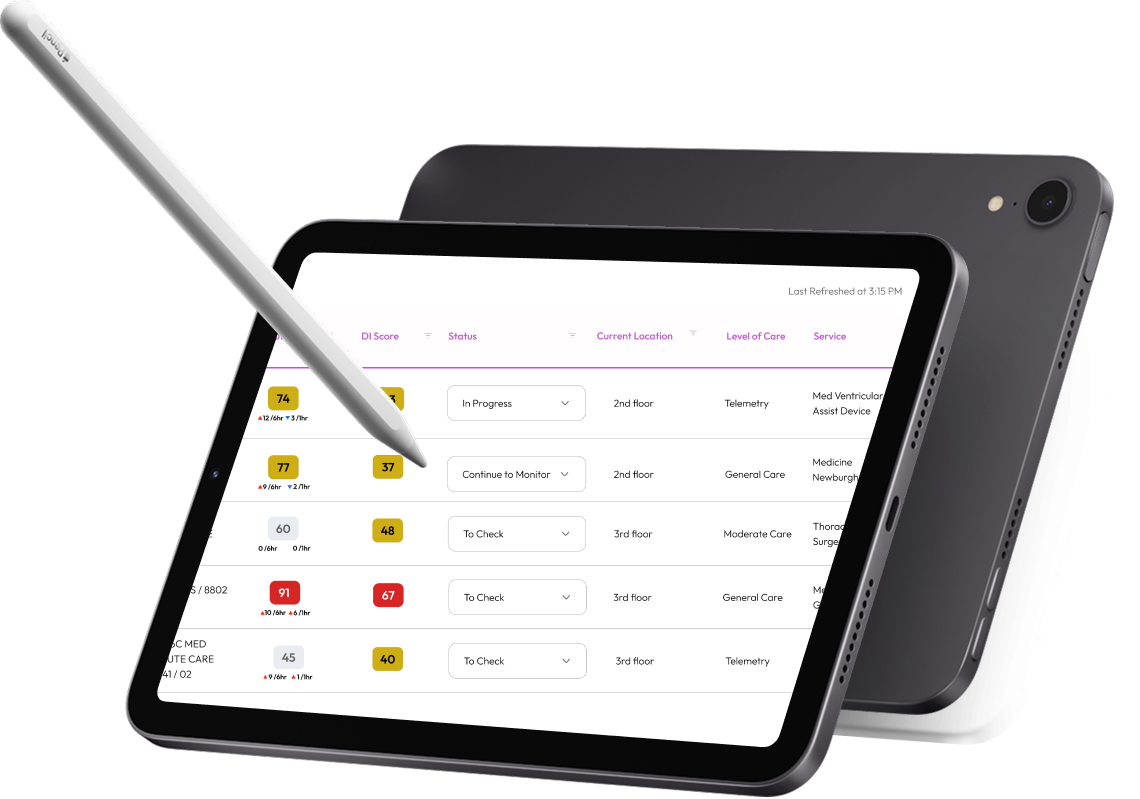
Clinical Decision Support Prototype in EHR
This project is under a Non-Disclosure Agreement.
Illustrative images, blurred for confidentiality.
Context
To address delays in clinical intervention, a predictive risk assessment model was developed to flag at-risk patients in advance. Initially tested with a response team, the tool was envisioned to scale across different care settings to strengthen early intervention. To be effective, however, it required more than algorithmic accuracy: it needed a thoughtful blend of human-centered design and systems thinking to integrate seamlessly into the electronic health record (EHR). The design goal was to reduce clinician cognitive load and support timely decision-making.
Our Goal
To design a clinician-friendly predictive risk interface that integrates seamlessly into the EHR, reduces cognitive load, and supports timely, informed decision-making across care settings.
Our Response
We partnered closely with clinical stakeholders to translate a predictive risk concept into a clearer, more intuitive decision-support interface. Using workflow mapping, iterative prototyping, and usability testing, we identified points of cognitive load and ambiguity, and refined how key signals were surfaced to clinicians. The resulting design aligned more naturally with existing clinical workflows, supported earlier situational awareness, and reduced the effort required to interpret patient risk across care settings.
Project Details
Working Team: Innovation Team, Data Analysts, Project Managers UX Lead
Stakeholders: Primary Investigators, EHR team, Clinicians, Hospitalists
Timeline: 1 year
Scope: UX Research, UX Design, Interface Design, Stakeholder Collaboration
My Role: User Experience Designer, Usability Specialist, Project Manager, Prototype Designer
Focus: Concept validation, prototype evaluation, usability testing, and insight synthesis
Testing & Research (2 Rounds)
Round 1 : Concept & Prototype Evaluation
Methods: Contextual Interviews, Concept Testing, Prototype Walkthroughs, Behavioral Observation
Tools: Zoom, Miro
Round 2: Usability Testing & Refinement
Methods: Task-Based Usability Testing, Feedback Synthesis, Iterative Validation
Tools: Zoom, Miro
Synthesis & Analysis
Methods: Empathy Maps, Thematic Analysis, Affinity Mapping
Tools: Miro
Interaction Support
Methods: Sketching, Wireframing, Low- to Mid-Fidelity Prototyping
Tools: Paper Prototypes, Figma
Key Project Highlights
Scalability
The model needed to be scalable to accommodate the distinct needs of various clinical units, such as adult and pediatric departments.
2. Risk and Protective Factors
Participants reported higher trust and usability when risk and protective factors were simplified in the UI.
3. Different preferences
Testing confirmed preferences around data display, visual cues, and iconography, shaping refinements for future iterations.
4. Confusion
Usability sessions surfaced areas of confusion, e.g., data value displays) and highlighted opportunities for iteration prior to broader rollout.
Design Process
-
Usability Testing (2 Rounds)
Conducted a moderated usability evaluation using a think-aloud protocol to assess the clarity and usability of key interface components. Sessions with clinicians and nurses focused on how users interpreted information, interacted with interface patterns, and navigated core UI behaviors.
-

Empathy Maps
Created five distinct empathy maps to capture variations in user needs, goals, and motivations across different roles. These maps highlighted how intentions and responsibilities shaped expectations and interactions with the interface.
-

Thematic Analysis
Conducted thematic analysis of interview data, organizing insights into tagged categories to support pattern recognition and deeper analysis.
-

Design Findings
Through thematic analysis of user interviews and synthesis of user and stakeholder feedback, we identified recurring patterns in how users interpret information, prioritize signals, and make sense of system output.
-

Design Insights
By analyzing these patterns, we uncovered insights related to cognitive load, mental models, and information prioritization that influenced how users understood and acted on presented information.
-

Design Principles
Based on the synthesized findings and insights, we established design principles to guide the next iteration of prototyping, focusing on surfacing only the most essential information needed for interpretation.
-

Sketching and Ideation
Led a stakeholder sketching workshop using note-taking, idea writing, Crazy 8s, and Big Idea synthesis to explore concepts and align on design direction.
-

Mid-Fidelity Prototyping
Translated outputs from the sketching workshop into mid-fidelity prototypes to explore structure, hierarchy, and interaction patterns. Prototyping decisions were informed by platform constraints and standard system capabilities, requiring close alignment with available tooling and asynchronous validation where direct stakeholder access was limited.
-

Stakeholder Engagement (Tech Team)
Engaged with platform stakeholders to understand system constraints, dependencies, and implementation considerations that informed design decisions.
-

Stakeholder Feedback on Mid-Fidelity Wireframes
Conducted mid-fidelity wireframe walkthroughs and feedback sessions with stakeholders to validate design direction, surface constraints, and inform iterative refinement.
Usability Testing Outcomes
Navigation efficiency
Clinicians completed critical patient data tasks significantly faster with the prototype compared to baseline workflows.
Adoption readiness
Users did not have any peer support and would usually train alone.
Validated design directions
Contextual inquiry through in-person observation of user environments.
Interface insights
Feedback from proxy users, peers, experts and stakeholders
Key Takeaways
-
Adapting to systemic constraints
During the presentation of the wireframes to the team responsible for integrating the model into the existing electronic health system, I encountered significant system constraints. This challenge forced me to pivot and adjust my design approach to align with the technical limitations, ensuring that the integration process would be seamless and efficient.
-
Translating qualitative insights to quantitative results
I primarily used qualitative methods and design thinking approaches, however, I needed to translate the findings into a format that could be understood by data scientists, researchers, and clinical stakeholders, ensuring that the results were actionable and accessible to all involved.
-
Embracing Project Shifts
After presenting the report to both my immediate team and the EHR system team, it was revealed that the project had been reprioritized and rescheduled for 2025. While not every project reaches its conclusion as initially planned, this shift offered an opportunity to reflect on the progress made and anticipate future adjustments.